EASD has highlighted a paper in Diabetologia and just published a short summary on their EASD learning website. Please see below. Copy the whole www into your browser
https://easd-elearning.eu/index.html@p=27062024.html
Unlocking AI’s potential to screen for type 1 diabetes
27th June 2024
Artificial intelligence is going to revolutionise also the medical field, especially when it comes to harnessing existing data sets for practical applications. A Swedish consortium has now published its approach to developing an AI-based population-wide screening strategy for type 1 diabetes. However, their proposal goes beyond mere disease prediction.
Since the world’s first insulin was injected into a human a century ago, efforts focused mainly on improving insulin treatment for diagnosed patients. Today, preventive therapy is being researched as the next milestone, and an increasing number of countries are discussing strategies to identify the target population for such treatments. To this end, existing data sets from observational cohort studies can be used together with known risk predictors such as islet autoantibodies, human leukocyte antigen (HLA) haplotypes and genetic risk scores. The challenge now is to translate this knowledge into effective screening strategies.
A recent “For Debate” article published in Diabetologia highlights the potential of artificial intelligence (AI) to transform the landscape of type 1 diabetes (T1D) screening and early diagnosis. The article summarises the position of several researchers and clinicians active in the field, who met in an open forum organised by the ASSET partnership, sponsored by the Swedish Innovation Agency. ASSET also emphasises the importance of AI for developing holistic screening strategies that extend beyond disease prediction.
From prediction to prevention
The ASSET initiative is taking a broad approach, focusing on AI to help inform screening programmes, test preventive therapeutics in a clinical setting, and evaluate the ‘implementability’ of such practices in healthcare systems,” the consortium sums up the outline of the project in their statement. As a first step, ASSET is building a machine learning pipeline based on data from the TEDDY cohort, which includes 8,640 high-risk children from birth to the age of 15 or with diagnosis of T1D. Once completed, their model will need to face an unseen data set and comparison with clinical outcomes to assess its sensitivity and specificity.
“AI has significant potential to revolutionise screening for autoimmune diseases, including T1D, by analysing vast amounts of data to identify patterns and risk factors that might not be apparent through other methods,” says Pedro F. Teixeira, first author of the paper. Gun Forsander, EASD member and co-senior author, adds: “Integrating AI in screening programmes could lead to more personalised monitoring strategies and enhance the operational feasibility, cost-effectiveness, and acceptance of such programmes at the population level. Early detection and individualised monitoring of affected individuals should prove effective in providing timely interventions, which may prevent or delay the onset of the disease.” Thus, a proactive approach driven by AI-based strategies should also be helpful in reducing T1D-related complications.
Four areas for AI in T1D prevention
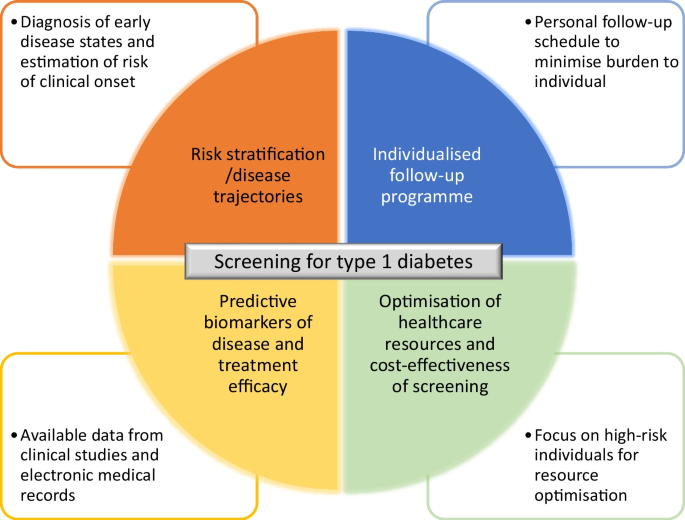
To contribute to the vision of preventive diabetes care, ASSET has identified four areas where AI can be applied, outlining the broad scope from T1D screening to potential future treatment approaches: (1) risk stratification, (2) individualised follow-up programmes, (3) identification of predictive and treatment efficacy markers, and (4) optimisation of healthcare resources and cost-effectiveness of screening
 Fig. 1: Artificial intelligence (AI) could be a key driver in the prevention of type 1 diabetes (T1D) in the future. The Swedish ASSET consortium has identified four areas where AI can be applied to provide an effective screening strategy for T1D (adapted from Teixeira et al., 2024).
Fig. 1: Artificial intelligence (AI) could be a key driver in the prevention of type 1 diabetes (T1D) in the future. The Swedish ASSET consortium has identified four areas where AI can be applied to provide an effective screening strategy for T1D (adapted from Teixeira et al., 2024).
In this broad approach, AI can be used to identify individuals at risk of developing T1D or in the early stages of the disease by assessing genetic susceptibility, family history, environmental exposures, and behavioural factors. It can also predict disease progression, differentiate between slow and fast progressors, and provide personalised intervention suggestions for clinicians, thereby optimising the use of healthcare resources. Finally, AI may lead to the identification of new markers or provide valuable insights into clinical trial design and population selection, thus supporting research into predictive drug development. Taken together, the authors state that these multiple opportunities offered by AI-based screening design could help lay the foundation for a precision medicine approach to T1D.
Balancing gains and challenges
“Finding individuals at risk for the disease allows them to be monitored, to be involved in clinical trials of preventive therapeutics and, in the worst case, to be prepared for a diagnosis avoiding an acute clinical presentation,” the ASSET consortium highlights the benefits of timely screening. However, “both operational and ethical considerations need to be taken into account before implementing the proposed technology on a large scale,” Teixeira points out.“The key issue,” says Åke Lernmark,
EASD member and second co-senior author, “is whether AI would allow the research community, together with industry, to capitalise on large publicly available data repositories to design screening programmes not only for the early detection of individuals at high risk, but also to identify tailored preventive therapies.”Overcoming the various challenges will require extensive collaboration between researchers, clinicians, and AI experts, as well as rigorous validation of AI models in order to gain acceptance not only from the target population but also from healthcare providers, regulatory authorities, payers and other relevant stakeholders, the authors conclude on the many dimensions taken on by their ambitious project.
To read this paper as full pdf free visit:
Free pdf
https://link.springer.com/article/10.1007/s00125-024-06089-5
Assisting the implementation of screening for type 1 diabetes by using artificial intelligence on publicly available data
Abstract
The type 1 diabetes community is coalescing around the benefits and advantages of early screening for disease risk. To be accepted by healthcare providers, regulatory authorities and payers, screening programmes need to show that the testing variables allow accurate risk prediction and that individualised risk-informed monitoring plans are established, as well as operational feasibility, cost-effectiveness and acceptance at population level. Artificial intelligence (AI) has the potential to contribute to solving these issues, starting with the identification and stratification of at-risk individuals.
ASSET (AI for Sustainable Prevention of Autoimmunity in the Society; www.asset.healthcare) is a public/private consortium that was established to contribute to research around screening for type 1 diabetes and particularly to how AI can drive the implementation of a precision medicine approach to disease prevention. ASSET will additionally focus on issues pertaining to operational implementation of screening. The authors of this article, researchers and clinicians active in the field of type 1 diabetes, met in an open forum to independently debate key issues around screening for type 1 diabetes and to advise ASSET.
The potential use of AI in the analysis of longitudinal data from observational cohort studies to inform the design of improved, more individualised screening programmes was also discussed. A key issue was whether AI would allow the research community and industry to capitalise on large publicly available data repositories to design screening programmes that allow the early detection of individuals at high risk and enable clinical evaluation of preventive therapies. Overall, AI has the potential to revolutionise type 1 diabetes screening, in particular to help identify individuals who are at increased risk of disease and aid in the design of appropriate follow-up plans. We hope that this initiative will stimulate further research on this very timely topic.
Introduction
Type 1 diabetes is commonly regarded as an autoimmune condition that starts long before symptomatic manifestations [1]. When reduced endogenous insulin production and hyperglycaemia reach a critical threshold, individuals develop symptoms and are sometimes diagnosed in dramatic circumstances when presenting in diabetic ketoacidosis (DKA).
Insulin replacement therapy has been available to treat type 1 diabetes for 100 years, with the last 30 years witnessing the development of more efficacious insulins, more accurate insulin delivering methods and more sophisticated ways to monitor blood glucose [2]. While insulin is a life-saving treatment, it is not a cure. Therefore, every child or adult that is diagnosed with type 1 diabetes has to come to terms with a complicated and potentially dangerous treatment regimen and faces the negative long-term medical, social and economic consequences of the disease [3,4,5]. Even though remarkable improvements in disease management and survival have been observed during the past century, mortality rate in type 1 diabetes is still two to eight times higher than in populations without diabetes. This is reflected in a loss of life expectancy at age 20 of approximately 12 years [6].
The holy grail of type 1 diabetes clinical research is to find treatments that prevent or delay the clinical onset of disease [7]. Similar to the success of antiretroviral drugs for the treatment of HIV infection, disease-slowing treatments need to be developed for individuals with presymptomatic type 1 diabetes. A number of large observational cohort studies have followed thousands of children from birth. A wealth of information on genetics (e.g. human leukocyte antigen [HLA] genes) and biomarkers (e.g. diabetes-related autoantibodies) in type 1 diabetes, as well as on the natural history of type 1 diabetes progression, has been obtained to identify risk factors for the pathogenesis leading up to the clinical disease [8,9,10,11,12]. Presymptomatic screening has been advocated for genetic and serological risk variables.
Early screening allows individuals at risk and their families to prepare for a diagnosis of type 1 diabetes, although advanced knowledge of disease risk may increase the psychological burden if there is no preventive treatment or possibility of enrolling in a clinical trial [13]. Screening has also reduced the occurrence of DKA and the risk and duration of hospitalisation at diagnosis and may provide positive long-term effects on the course of the disease [14, 15]. The experience in Finland suggests that participation in prospective follow-up studies reduces the frequency of DKA in children at diagnosis of type 1 diabetes, but that genetic screening alone does not decrease DKA risk [16]. This highlights the need for predictive biomarkers and sequential follow-up of autoantibody-positive individuals. The ultimate goal is to prevent clinically overt type 1 diabetes (stage 3) by providing effective and safe treatments for individuals at high risk for the disease but still with sufficient beta cell function. These could be pharmacological interventions targeting the immune system, to replenish lost beta cells, or advanced therapies using stem cells and gene editing [13, 17, 18].
While advances in screening and prevention have been acknowledged, improvements are needed in the areas of risk prediction, operationality of screening programmes, health-economic evaluation and interactions with societal stakeholders for practical implementation.
Conclusion
Effective screening of type 1 diabetes risk in the general population would be beneficial for affected individuals and their families, academic researchers and pharma developing preventive therapeutics. Type 1 diabetes is a heterogeneous disease with distinctively progressive hallmarks that makes it amenable to a risk-based screening approach. Finding individuals at risk for the disease allows them to be monitored, to be involved in clinical trials of preventive therapeutics and, in the worst case, to be prepared for a diagnosis, avoiding an acute clinical presentation. Once treatments are available, screening will allow healthcare providers to select individuals who would benefit from a specific intervention. The design of screening programmes, including variables to screen for, how often to screen and how long to screen for, are questions that can be addressed using AI (Fig. 2). The application of AI to develop screening programmes, from identifying biomarkers that predict disease trajectory to identifying the appropriate timing of monitoring and determining cost-effectiveness, is still in its infancy. Current examples of AI application in diabetes include screening for diabetes complications and predicting hospitalisation for DKA [55, 56]. The potential benefits of AI should be weighed against the drawbacks, such as issues around data sharing, ethics and possible biases, before any AI-driven clinical support tools are introduced in population screening programmes.
Areas where AI could help drive the implementation of screening for type-1 diabetes
The ASSET initiative is taking a broad approach, focusing on AI to help inform screening programmes, testing preventive therapeutics in a clinical setting, and evaluating the ‘implementability’ of such practices in healthcare systems. ASSET provides the means to link experts in clinical type 1 diabetes research with industry, ethics boards and public healthcare to jointly capitalise on publicly available databases for designing screening programmes, identifying individuals at risk and assisting with the use of precision medicine in personalised clinical prevention trials.
Nyhetsinfo
www red DiabetologNytt