Diabetes typ 2 är vanligare hos män som genomgått tidig pubertet, visar en studie vid Göteborgs universitet. Låg pubertetsålder hos män kan också kopplas till ökad risk för att sjukdomen, om den utvecklas, kräver insulinbehandling.
Den aktuella observationsstudien, publicerad i tidskriften Diabetologia, omfattar 30 697 män i Sverige födda 1945-1961. Uppgifter om deras pubertetsålder och BMI före och efter puberteten hämtades från en populationsbaserad epidemiologisk studie, The BMI Epidemiology Study Gothenburg.
Underlaget omfattade BMI-värden vid 8 och 20 års ålder, samt pubertetsålder definierad som den tidpunkt då längdtillväxten varit som snabbast, alltså mitt i spurten, med en snittålder på 14 år. Till detta adderades sedan nationella hälsodata från svenska register. Genomsnittlig uppföljningstid var 30 år, från 30 års ålder och framåt.
I hela gruppen var det 1 851 män, ungefär sex procent, som fick diagnosen typ 2-diabetes under uppföljningstiden. Snittåldern för diagnos var drygt 57 år, vilket i studien utgör gräns för vad som beskrivs som tidig respektive sen typ 2-diabetes.
Tydligt förhöjda risker
Den aktuella studien slår inte fast några orsakssamband, och klarlägger inte heller några mekanismer mellan tidig pubertet och typ 2-diabetes. Resultaten är dock tydliga, och kvarstår även efter justering för BMI i barndomen.
Starkast var kopplingen mellan tidig pubertet och tidigt diagnosticerad typ 2-diabetes, som utvecklades före 57 års ålder. Den fjärdedel av studiedeltagarna som hade tidigast pubertetsålder (vid cirka 9-13 års ålder) löpte fördubblad risk att drabbas jämfört med den fjärdedel som hade högst ålder vid sin pubertetsspurt (cirka 15-18 år). Detta efter justering för deltagarnas BMI vid 8 års ålder. Sambandet mellan tidig pubertet och tidigt utvecklad typ 2-diabetes kvarstod även efter justering för BMI vid 20 års ålder.
Risken för sen typ 2-diabetes, efter 57 års ålder, var också förhöjd i gruppen deltagare som genomgått tidig pubertet, men den kopplingen var inte lika stark, och kvarstod inte efter justering för BMI vid 20 års ålder.
Det faktum att deltagare som genomgått tidig pubertet oftare behandlades med insulin i de fall sjukdomen utvecklades, framkom via data från register över förskrivna läkemedel, och styrker resultaten.
Viktigt att följa och hjälpa
Bakom studien står docent Jenny Kindblom och professor Claes Ohlsson med kollegor på Sahlgrenska akademin vid Göteborgs universitet.
– Vår slutsats är att tidig pubertet kan ses som en ny och oberoende riskfaktor för typ 2-diabetes hos män. Risken är uppenbart högre bland dem som varit tidig i sin pubertet, och vi uppskattar att 15 procent färre män som fick diagnosen under studien skulle ha utvecklat typ 2-diabetes om de inte hade genomgått puberteten så tidigt, säger Jenny Kindblom, och fortsätter:
– Fynden stärker bilden av att tidig pubertet kan ge negativa effekter, och att ett högt BMI både före och efter puberteten bidrar. För att identifiera och hjälpa fler individer är det därför viktigt med kontinuerlig kontroll av längd- och viktutveckling, inte bara barndomen utan även i tonåren, avslutar hon.
Titel: Early puberty and risk for type 2 diabetes in men
https://link.springer.com/article/10.1007%2Fs00125-020-05121-8
Bilder: Genrebild från Matton images och porträttbild på Jenny Kindblom (foto: Cecilia Hedström)
Av Margareta Gustafsson Kubista
Press release från Sahlgrenska Akademin, Göteborg
ABSTRACT
Early puberty and risk for type 2 diabetes in men
Diabetologia (2020)Cite this article
Abstract
Aims/hypothesis
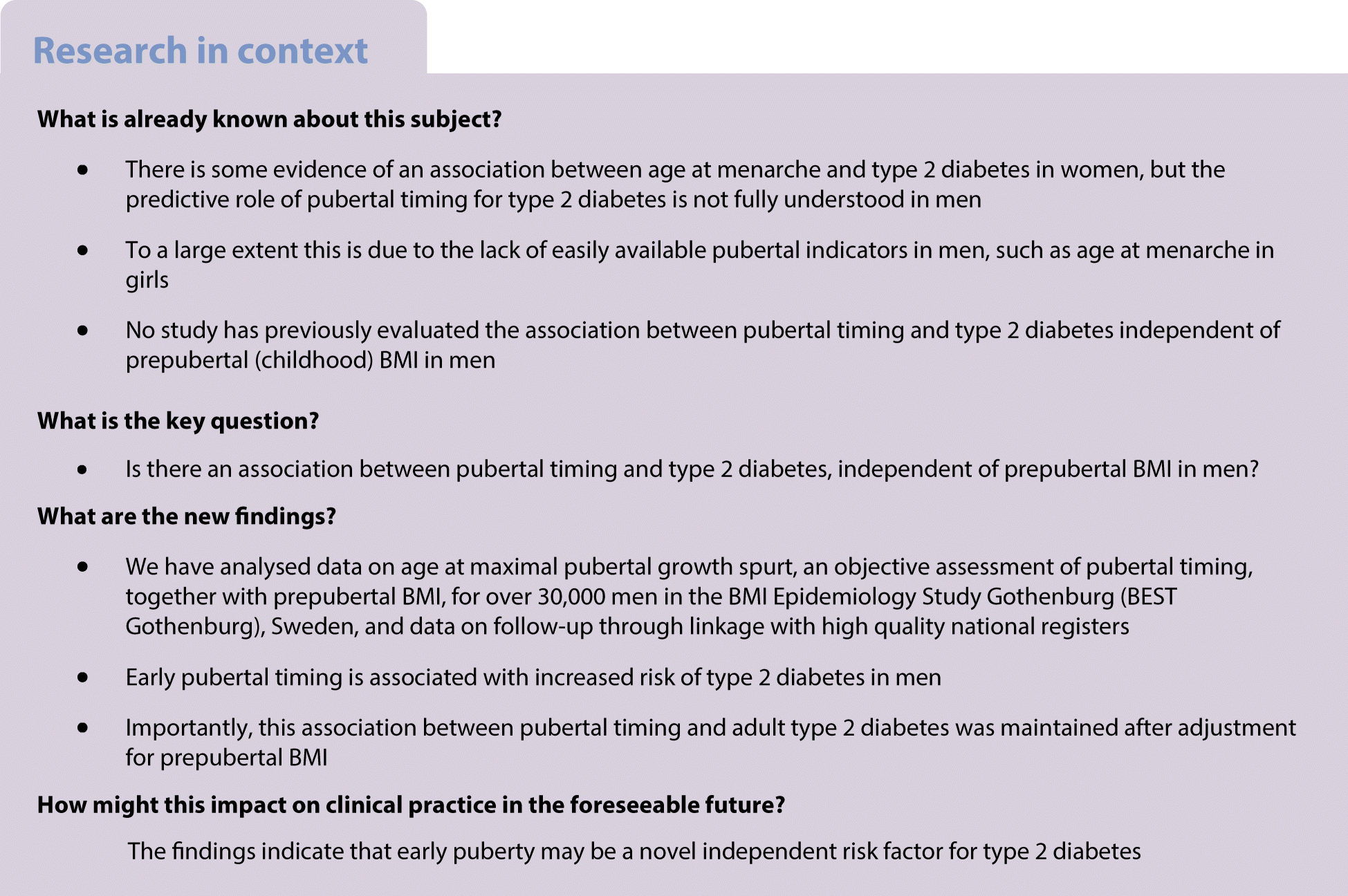
The association between pubertal timing and type 2 diabetes, independent of prepubertal BMI, is not fully understood. The aim of the present study was to evaluate the association between pubertal timing and risk of adult type 2 diabetes, independent of prepubertal BMI, in Swedish men.
Methods
We included 30,697 men who had data for BMI at age 8 and 20 years and age at Peak Height Velocity (PHV), an objective assessment of pubertal timing, available from the BMI Epidemiology Study Gothenburg (BEST Gothenburg), Sweden. Information on type 2 diabetes (n = 1851) was retrieved from the Swedish National Patient Register. HRs and 95% CIs were estimated by Cox regression analysis. We observed violations of the assumption of proportional hazards for the association between age at PHV and the risk of type 2 diabetes and therefore split the follow-up period at the median age of type 2 diabetes diagnosis (57.2 years of age) to define early (≤57.2 years) and late (>57.2 years) type 2 diabetes diagnosis.
Results
Age at PHV was inversely associated with both early (HR 1.28 per year decrease in age at PHV, 95% CI 1.21, 1.36) and late (HR 1.13, 95% CI 1.06, 1.19) type 2 diabetes. After adjustment for childhood BMI, the associations between age at PHV and both early (HR 1.24, 95% CI 1.17, 1.31) and late (HR 1.11, 95% CI 1.05, 1.17) type 2 diabetes were similar. Moreover, early age at PHV predicted insulin treatment of type 2 diabetes (OR 1.25 per year decrease in age at PHV, 95% CI 1.17, 1.33). Assuming a higher risk among those with an age at PHV below the median, the population attributable factor indicates that 15% fewer of the diagnosed individuals would have developed type 2 diabetes had they not reached puberty early.
Conclusions/interpretation
These findings indicate that early puberty may be a novel independent risk factor for type 2 diabetes.
Läs hela artrikeln i sin helhet som pdf utan lösenord
https://link.springer.com/article/10.1007%2Fs00125-020-05121-8
Some issues from the article
Introduction
With the global rise in the prevalence of type 2 diabetes, identification of early risk factors that predispose individuals to type 2 diabetes is a priority. The strong association between a high adult BMI and risk of type 2 diabetes is well established, and prevention of adult obesity remains among the most important measures to reduce the burden of type 2 diabetes [1, 2]. We and others have recently demonstrated that being overweight during childhood and BMI change during puberty are associated with type 2 diabetes [3, 4]. These findings indicate that the increased risk of diabetes associated with elevated BMI may already be present in childhood and adolescence.
In addition to high BMI during childhood and adolescence, a few studies have indicated that early puberty is associated with increased risk of type 2 diabetes in women [5,6,7,8,9]. Information on age at menarche is often available and used as an estimate of pubertal timing in women, and recalled age at menarche has been shown to correlate rather well with actual age at menarche [10,11,12]. One study from the UK demonstrated that individuals with recalled age at menarche above the median had a lower risk of type 2 diabetes compared with those with recalled age at menarche below the median [8]. Recently, using the large amount of data available through the UK Biobank study, women with menarche before 11 years of age (20.2%) were found to have 76% higher risk of type 2 diabetes than those aged between 11 and 15 years at menarche [5]. Given the clear inverse association between childhood BMI and age at menarche in women [13,14,15,16,17], adjustment for the confounding effect of prepubertal BMI is important. Only one study, which analysed data on 1381 women in a British birth cohort born in 1946, had data available for prepubertal height and weight and was able to adjust for childhood BMI. In that study, the association between age at menarche and type 2 diabetes was strongly attenuated and no longer significant after adjustment for BMI at 7 years of age [9].
For boys, retrospective studies of pubertal timing are hampered by the lack of easily available pubertal indicators. In the UK Biobank study, recalled age at voice breaking is available as a pubertal marker [5]. The three self-reported categories of voice breaking in that study were ‘younger than average’, ‘about average’ and ‘later than average’, and the results showed higher risk for type 2 diabetes for the 4.3% who reported early voice breaking (OR 1.44, 95% CI 1.3, 1.59) and lower risk for the 5.9% who reported late voice breaking (OR 0.69, 95% CI 0.61, 0.77) compared with the approximately 90% that reported age at voice breaking ‘about average’ [5]. Age at voice breaking when reported by recall in adult life has not been validated [18]. Importantly, the analyses in the UK Biobank study could not be adjusted for prepubertal BMI, which is known to influence pubertal timing in men [19]. Therefore, the association between pubertal timing and type 2 diabetes, independent of prepubertal BMI, is unknown in men [5].
In the ongoing BMI Epidemiology Study Gothenburg (BEST Gothenburg), Sweden, both age at pubertal timing and information on childhood BMI and young adult BMI are available for a cohort of men born between 1945 and 1961. We used a modified Infancy-Childhood-Puberty model [20] to calculate age at peak height velocity (PHV), an objective assessment of pubertal timing, in men. Using these data, we have recently demonstrated an inverse association between prepubertal BMI at age 8 and age at PHV [19], and we also observed a clear secular trend towards earlier age at PHV in males from the 1940s up to the present [21].
In the present cohort study, we hypothesised that early age at PHV, independent of prepubertal BMI, is associated with increased risk of type 2 diabetes in men. The aim of the present study was to evaluate the association between pubertal timing and risk of adult type 2 diabetes, independent of childhood BMI, in Swedish men.
Discussion
Childhood BMI is a known predictor of type 2 diabetes risk in men, but the predictive role of pubertal timing, independent of prepubertal BMI, for adult type 2 diabetes is not fully understood. We have collected information on height before, during and after puberty and used this data to calculate age at PHV, an objective assessment of pubertal timing, for 30,697 men in the BEST Gothenburg study. Using this data, we have demonstrated an inverse association between objectively assessed pubertal timing and the risk of type 2 diabetes in men. Importantly, we were able to adjust for childhood BMI at 8 years of age and show that the associations between pubertal timing and both early and late adult type 2 diabetes are independent of prepubertal BMI.
Male pubertal timing is not well studied. For girls, an inverse association between childhood BMI and age at menarche has been identified [17] and studies have established a secular trend of earlier menarcheal age since the mid-nineteenth century [30], partly explained by increased childhood BMI during the last 60 years [31]. Retrospective studies of male puberty are limited by the lack of easily available pubertal indicators, therefore, less is known regarding the determinants and the consequences of male pubertal timing. We have collected retrospective growth data, calculated age at PHV according to a modified infancy–childhood–puberty model [20] and used it as an objective assessment of pubertal timing in boys, as previously described [19, 21, 25]. Age at PHV is the age at the time of the maximum growth spurt, which occurs approximately 2 years after pubertal onset in boys [32]. Using age at PHV we recently reported a secular trend for pubertal timing from the 1940s onwards [21] and we have also demonstrated an inverse association between prepubertal childhood BMI and age at PHV [19]. In the current study we demonstrate that early age at pubertal timing is associated with increased risk of adult type 2 diabetes, independent of childhood BMI, in Swedish men.
The studies using age at menarche as assessment of pubertal timing suggest a risk pattern associated with early pubertal timing in women, including increased risk of type 2 diabetes and cardiovascular disease [5,6,7,8,9, 33, 34]. Among the studies in women we only found one that was able to adjust the association between early age at menarche and type 2 diabetes for prepubertal childhood BMI. The results indicated that the association was strongly attenuated by adjustment for prepubertal BMI and was no longer significant after the adjustment [9]. For men, the potential health consequences of early or late pubertal timing have not been evaluated in detail. In the UK Biobank study, self-reported age at voice breaking was inversely associated with the risk of type 2 diabetes. This finding is in line with the results using age at menarche in women in the same study [5], and with findings from previous studies demonstrating an association between early age at menarche and increased risk of type 2 diabetes [6,7,8,9]. The UK Biobank study looked at associations between extremes in self-reported pubertal timing (early-maturing [4.3%] and late-maturing [5.9%] boys) and risk of type 2 diabetes, and reported adverse health consequences for the 4.3% with self-reported early puberty [5]. In the present study, we demonstrate an inverse linear association between age at PHV, evaluated as a continuous variable, and the risk of type 2 diabetes. Importantly, as prepubertal BMI was not available in the UK Biobank study, the association between pubertal timing and type 2 diabetes in men could not be adjusted for childhood BMI [5] and, consequently, the association between pubertal timing and type 2 diabetes, independent of prepubertal BMI, is not known. As prepubertal BMI was available in the present study, we were able to demonstrate that age at PHV was associated with risk of type 2 diabetes independent of childhood BMI in men. This finding is further supported by the observation that age at pubertal timing was inversely associated with type 2 diabetes that required insulin treatment, i.e. type 2 diabetes with a worse global risk profile than those not requiring insulin treatment. Moreover, the notion that the significant inverse association between age at pubertal timing and risk of type 2 diabetes is also maintained after adjustment for education level and birthweight indicates that this association is robust to adjustment for available relevant confounders. Our analyses also demonstrated that late pubertal timing was associated with reduced risk of early type 2 diabetes, independent of prepubertal BMI.
The mechanisms behind the observed association between early pubertal timing and increased risk of type 2 diabetes in men are not clear. Since this is an observational study, we can only hypothesise on the possible factors mediating the observed association between early pubertal timing and increased risk of type 2 diabetes. The association between early menarche and increased risk of type 2 diabetes is reported to be completely [6, 8, 9] or partly [5, 7] attenuated by adjustment for adult age BMI, suggesting that increased adiposity might be an important mediator of the association in women. Some previous studies have shown a higher BMI and greater android fat mass at age 60–64 in men with earlier pubertal timing [18, 35], suggesting that pubertal timing may modulate BMI and adiposity during adult life in men. Unfortunately, BMI during middle age was not available in our study to test this hypothesis, but the notion that adjustment for young adult BMI at 20 years of age attenuated the association between pubertal timing and late type 2 diabetes aligns with the hypothesis that adult BMI could be partly involved in the mediation of this association. In a previous study, we demonstrated a higher amount of visceral adipose tissue in men with early puberty [25]. One may speculate that early puberty leads to the accumulation of visceral fat, and thereby increased cardiometabolic risk.
The limitations associated with the present study include the fact that information on BMI later in life was not available and that information on family history of diabetes and smoking was lacking. Another limitation is that the results may have limited generalisability to other ethnicities with a higher prevalence of type 2 diabetes, as Sweden and northwestern Europe have a low prevalence. Moreover, type 2 diabetes diagnoses were captured through hospital-based registers and it was not possible to verify a correct classification of the outcome diagnosis. However, the Prescribed Drugs Register captures all insulin dispensed at Swedish pharmacies and the strong association with insulin-treated type 2 diabetes supports a true association between pubertal timing and type 2 diabetes. The strengths of the study include that we used a well-powered population-based cohort with information on the objectively assessed pubertal timing and BMI available both before and after puberty, together with the long follow-up. Moreover, healthcare in Sweden is provided free of charge, which makes socioeconomic bias in diagnosis and representativeness unlikely.
In conclusion, we demonstrate that early pubertal timing is associated with increased risk of type 2 diabetes in Swedish men, independent of prepubertal BMI.
Nyhetsinfo
www red DiabetologNytt

