Dr. Roy Beck on CGM Accuracy and Use: “The benefit is far exceeding the burden now.”
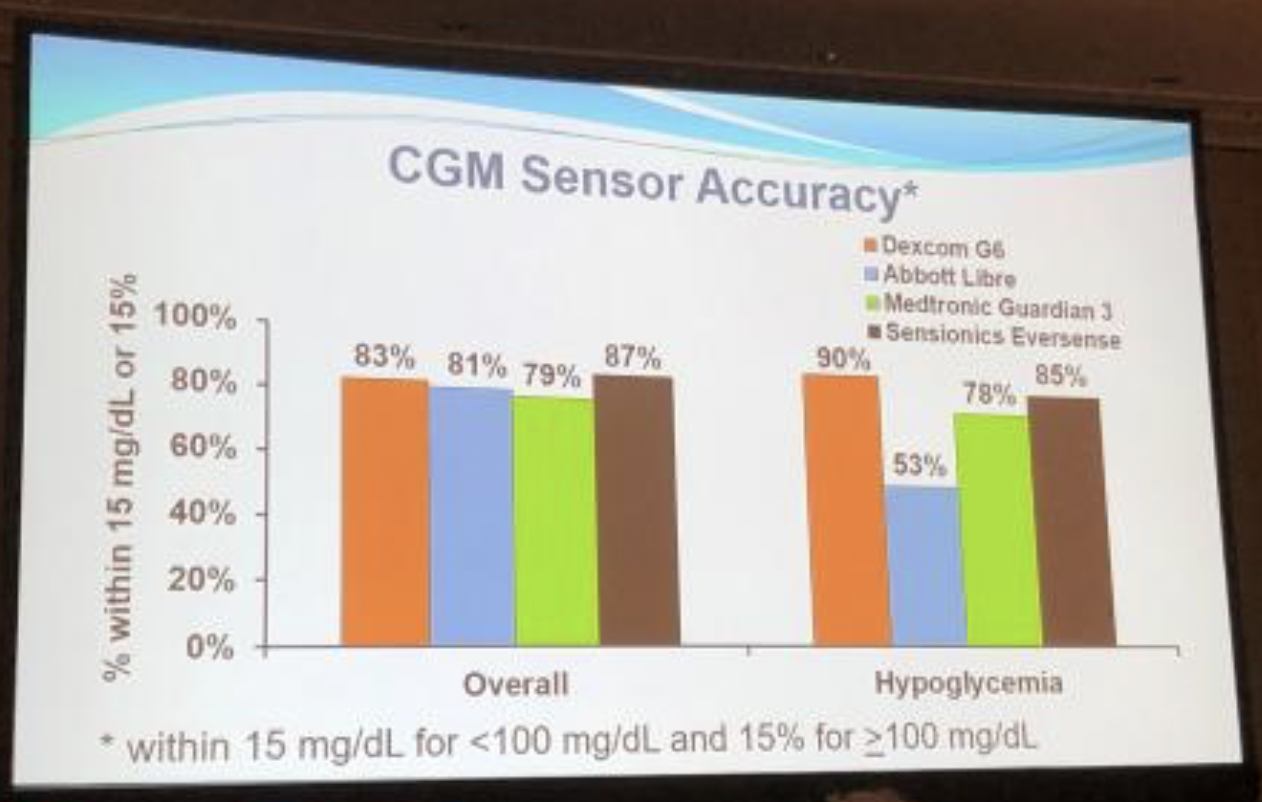
Jaeb Center’s Dr. Roy Beck provided a very positive overview of continuous glucose monitor (CGM) options in the US, covering the four available systems: Dexcom’s G6, Abbott’s FreeStyle Libre, Medtronic’s Guardian 3, and Senseonics’ Eversense.
We appreciated seeing the system-by-system accuracy stacked up side-by-side. The main takeaway: all four CGMs are pretty comparable on overall accuracy (left side of photo). There were some differences in accuracy of hypoglycemia (right side of photo), with the G6 being the most accurate in this study.
Dr. Beck concluded that CGM is becoming more widespread, and the future will see sensors that are smaller, disposable, and cheaper – facilitating more widespread use, particularly in type 2 diabetes.
Does When We Eat Matter? Effects of Timing on Weight, Metabolic Risk Factors, and Glycemic Control
Experts shared the latest data behind intermittent fasting and meal timing. This was one of the most crowded sessions of the day – highlighting the quickly growing interest surrounding meal timing and intermittent fasting!
The experts shared that time-restricted feeding (TRF) – eating in a narrower time period each day, typically within an 8-10 hour window – can improve health. The strongest evidence is from “early TRF”, e.g. eating from 8am -6 pm as opposed to 4pm - 2am, because it better aligns eating with the body’s circadian rhythm. Early TRF is associated with:
- Decreased hunger or food intake
- Weight loss
- Reduced glucose and insulin levels and improving insulin sensitivity
- Lowered blood pressure, and
- Increased fat oxidation (i.e., fat burning)
It was emphasized that TRF can be practiced with or without cutting calories. In addition, benefits are proportional to daily fasting duration; this means even small modifications in one’s eating produce results, but a longer fasting time may result in greater health benefits.
Experts stressed, however, that the benefits of changing meal timing do not outweigh the benefits of reducing processed food intake. Dr. Courtney Peterson from University of Alabama at Birmingham stated, “despite the evidence for the benefits of intermittent fasting, I still don’t subscribe to the ‘you can eat whatever you want’ theory.” Speak with your healthcare provider if you are interested in time-restricted feeding, as there may be necessary adjustments to your insulin requirements and diabetes medications.
Chiglitazar Reduces A1C in People with Type 2 Diabetes: Phase 3 Study Results
In two phase 3 studies in type 2 diabetes, chiglitazar proved to be safe and showed greater A1C reductions compared to placebo and comparable effects to sitagliptin (Januvia), a DPP-4 inhibitor. Chiglitazar is a PPAR Pan-Agonist that activates a protein that regulates genes involved in using fats for energy and decreasing insulin resistance.
In the CMAP trial comparing chiglitazar to placebo, both the 32 mg and 48 mg doses of chiglitazar showed a greater decrease in A1C lowering at 24 weeks than placebo. Over 24 weeks:
- The 32 mg dose of chiglitazar was associated with an A1C decrease of 1.3% (from a baseline A1C of 8.5%).
- The 48 mg dose of chiglitazar was associated with an A1C decrease of 1.5% (from a baseline A1C of 8.6%).
- The placebo group experienced an A1C decrease of 0.5% (from a baseline A1C of 8.6%).
In the CMAS trial comparing chiglitazar to Januvia, chiglitazar achieved similar A1C lowering to Januvia at 24 weeks. Over 24 weeks:
- The 32 mg dose of chiglitazar was associated with an A1C decrease of 1.4% (from a baseline A1C of 8.5%).
- The 48 mg dose of chiglitazar was associated with an A1C decrease of 1.5% (from a baseline A1C of 8.6%).
- Januvia was associated with an A1C decrease of 1.5% (from a baseline A1C of 8.6%).
Notably, chiglitazar proved to be safe for people with type 2 diabetes, with no difference in side effects compared to placebo or Januvia. In less positive news from the trial, chiglitazar was associated with slight weight gain (about 2.2lbs or 1 kg).
Cut the Higher Dose Pills in Half
Dr. Jean Francois-Yale from McGill University outlined how, in some instances, healthcare providers might prescribe the higher dose of an SGLT-2 inhibitor (or even a GLP-1 agonist) but tell people with diabetes to cut their dose in half. This leads to a lower copay for people with diabetes, a method that works because the higher and lower doses are the same price.
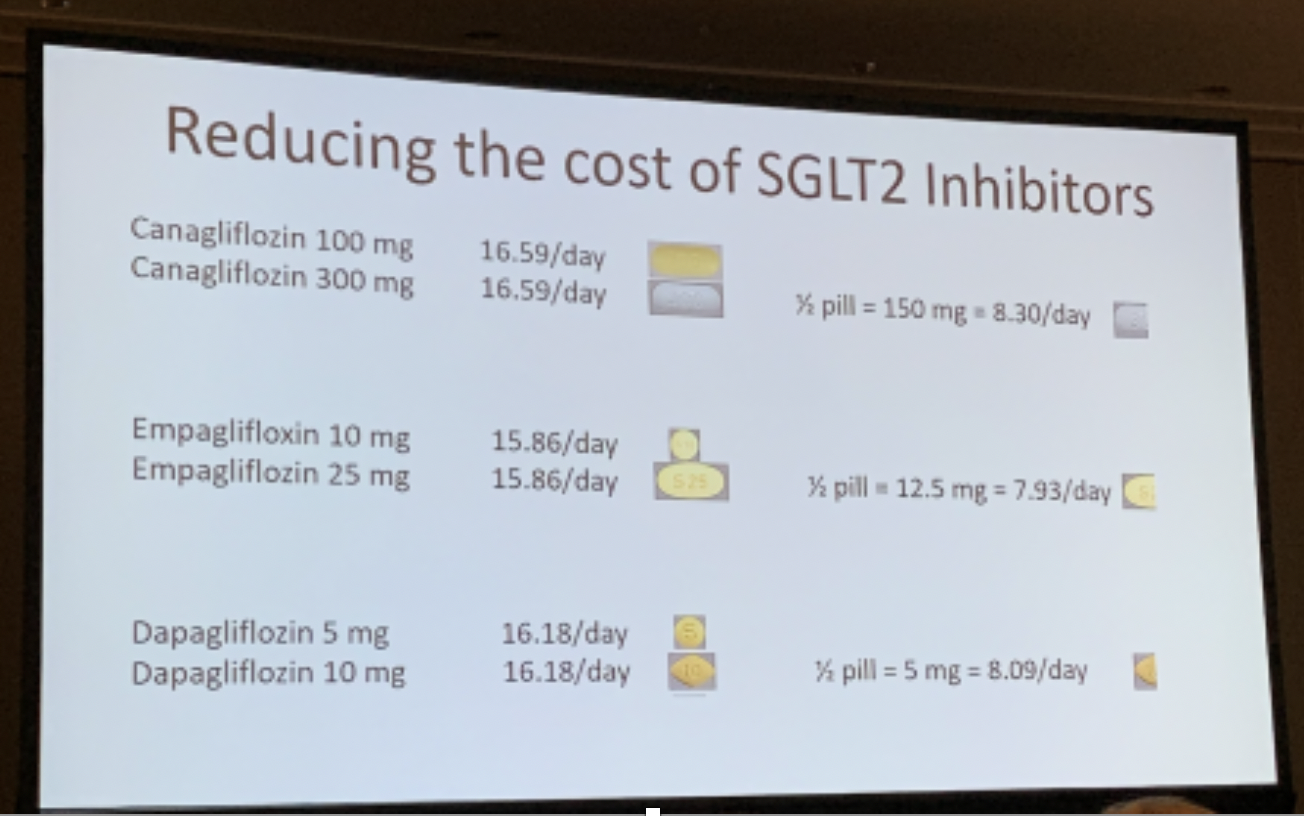
SGLT-2 inhibitors (eg. Invokana, Farxiga, Jardiance) and GLP-1 agonists (eg. Victoza, Trulicity, Ozempic) have been shown to reduce A1C, improve weight loss, and protect the heart and kidneys in people with type 2 diabetes. Dr. Francois-Yale turned to what is a big hurdle for some people for these types of drugs: cost. He detailed a simple yet novel strategy that he uses in practice that can make a dramatic difference for people with diabetes who are typically receiving the lower dose of the drug: cut high dose pills in half and take them separately. This effectively halves the price of their medication, but people with diabetes still get the dose of medicine they need.
Medtronic and Dexcom Have Become Official Tidepool Loop Partners!
 In new news, Medtronic announced that its Bluetooth-enabled alternate controller enabled (ACE) pump and Guardian Sensor 3 interoperable continuous glucose monitor (iCGM) will be compatible with the Tidepool Loop automated insulin delivery (AID) app. Medtronic’s Bluetooth-enabled ACE pump and Guardian Sensor 3 iCGM are both under development and not yet submitted to FDA. Dexcom has also partnered with Tidepool Loop to integrate its already-available G6 iCGM.
In new news, Medtronic announced that its Bluetooth-enabled alternate controller enabled (ACE) pump and Guardian Sensor 3 interoperable continuous glucose monitor (iCGM) will be compatible with the Tidepool Loop automated insulin delivery (AID) app. Medtronic’s Bluetooth-enabled ACE pump and Guardian Sensor 3 iCGM are both under development and not yet submitted to FDA. Dexcom has also partnered with Tidepool Loop to integrate its already-available G6 iCGM.
Tidepool Loop will be an automated insulin delivery app for iPhone and Apple Watch that connects to an insulin pump and CGM using Bluetooth and automatically adjusts the user’s basal rate with the goal to reduce high and low blood glucose.
Medtronic and Dexcom join Tidepool Loop’s first partner, Insulet’s Omnipod, leaving just Tandem, Abbott, and Senseonics as US players not yet on board. Tidepool Loop’s Medtronic and Dexcom partnerships are a huge step in developing devices that can be used together and increasing the number of options for people with diabetes.
From www.diatribe.org
Nyhetsinfo
www red DiabetologNytt
